micro-IDent® und micro-IDent®plus11
Ihre Testsysteme für die sichere Identifizierung von 5 bzw. 11 parodontopathogenen Markerkeimen
Parodontitis und Periimplantitis sind Infektionskrankheiten, die auf eine spezielle Gruppe von Bakterien zurückzuführen sind. Diese Markerkeime zerstören aktiv parodontales Weich- und Knochengewebe, führen zu massiven Entzündungsreaktionen und letztlich zum Verlust natürlicher Zähne und Implantate. Für eine langfristig erfolgreiche Therapie ist eine gezielte Bekämpfung dieser Bakterien von entscheidender Bedeutung. Markerkeimanalysen mit micro-IDent® und micro-IDent®plus11 geben Auskunft über Vorkommen und Konzentration von 5 bzw. 11 parodontopathogenen Spezies und deren Zugehörigkeit zu „Bakterienkomplexen“. Die Testergebnisse sind die optimale Grundlage für eine individualisierte Therapieplanung. Sie ermöglichen dem behandelnden Zahnarzt die Auswahl adjuvanter Antibiotika ebenso wie die Festlegung sinnvoller Recall-Intervalle und die Dokumentation des Behandlungserfolges.
Optimale Behandlungssicherheit auf Basis von Markerkeimanalysen
Entzündungen des Parodontalgewebes und fortschreitender Knochenabbau sind Folgen einer Infektion durch parodontopathogene Markerkeime. Für eine zielgerichtete und erfolgreiche Parodontaltherapie ist die Elimination bzw. deutliche Reduktion dieser Markerkeime von zentraler Bedeutung. Da die Zusammensetzung der Subgingivalflora individuell stark variiert, ist eine gezielte Behandlung nur auf Basis einer Analyse des Keimspektrums möglich. Erst das Wissen um Zusammensetzung und Höhe der Bakterienbelastung ermöglicht die Planung einer optimalen individuellen Behandlungsstrategie mit minimalem Einsatz von Antibiotika. Markerkeimanalysen mit micro-IDent® und micro-IDent®plus11 helfen so bei der evidenzbasierten Auswahl eines optimal wirksamen Medikamentes und tragen damit zur Vermeidung von Therapiefehlern oder ineffizienten Therapieformen bei. Regelmäßige Kontrolluntersuchungen zur Überprüfung des Behandlungserfolges und zur Früherkennung von Reinfektionen im Recall helfen das klinische Bild auch langfristig stabil zu halten. So ermöglicht eine diagnostisch fundierte Behandlung einen höheren therapeutischen Erfolg und folglich eine wachsende Zufriedenheit der Patienten.
Periimplantitis – Vorbeugen mit Markerkeimanalysen
Bei Vorliegen einer Periimplantitis führt eine durch Bakterien verursachte Entzündung des Weichgewebes zu Knochenabbau und letztlich zur Lockerung oder gar zum Verlust des Implantates. Das Keimspektrum bakteriell bedingter Infektionen ist dabei analog zu dem von Parodontalerkrankungen. Die für den Verlust der natürlichen Bezahnung verantwortlichen Keime gefährden so auch die erfolgreiche Eingliederung des Zahnersatzes. Die mikrobiologische Analyse ist folglich auch in der Implantologie ein wichtiges Werkzeug zur frühzeitigen Diagnostik und zielgerichteten Prävention. Auf Basis der Markerkeimanalysen mit micro-IDent® und micro-IDent®plus11 kann die Entscheidung getroffen werden, welche therapeutischen Maßnahmen für die Eradikation der individuellen Bakterienbelastung erforderlich sind. Die Eingliederung enossaler Implantate sollte erst nach erfolgreicher Keimreduktion bzw. -elimination erfolgen. Die im Vorfeld einer Implantation durchgeführte Analyse zeigt, ob ein geplanter Eingriff durch eine bestehende Bakterienbelastung bereits von vorneherein gefährdet ist. Erst eine negative Analyse signalisiert Keimfreiheit und gibt folglich grünes Licht für die implantatprothetische Versorgung. So erhalten Sie auf einfachem Weg optimale Behandlungssicherheit in Ihrem und im Interesse des Patienten.
Steigende Kosten im Gesundheitswesen führen zu ständig sinkenden Zuschüssen der Krankenkassen auch bei zahnärztlichen Leistungen und Zahnersatz. Ziel von Patient und Zahnarzt muss es daher sein, die Zähne möglichst lange gesund zu erhalten. Dabei helfen Markerkeimanalysen Risiken aufzuzeigen, bevor irreversible Schäden entstehen und kostspielige Behandlungen erforderlich werden. Vor umfangreichen prothetischen Sanierungen mit ebenfalls hohem finanziellem Aufwand geben unsere Testsysteme die Sicherheit, dass der Erfolg des Eingriffs nicht durch bestehende bakterielle Infektionen gefährdet ist. Sie helfen aber auch, Entzündungen an bereits eingesetzten Implantaten schnell und sicher zu diagnostizieren, damit eine angemessene Therapie eingeleitet werden kann.
 |
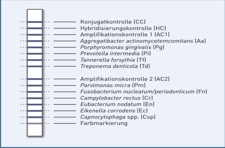 |
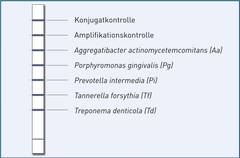
| micro-IDent® | micro-IDent®plus11 |
Markerkeimdiagnostik mit micro-IDent® und micro-IDent®plus11 auf einen Blick
Vorteile
- Quantitative, hochspezifische und -sensitive Bestimmung relevanter Markerkeime zur Optimierung von Behandlungsstrategie und Recall
- Kenntnis des Erregerspektrums ermöglicht die Wahl des richtigen Antibiotikums und sichert eine hohe Therapieerfolgsquote
- Kontrolluntersuchungen dokumentieren den Behandlungserfolg
- Untersuchungen im Recall erlauben die Früherkennung von Rezidiven
- Risikoeinschätzung vor aufwändigen Sanierungen schützt vor Implantatverlusten
Indikationen für Markerkeimanalysen
- Bei Parodontalerkrankungen mit Taschentiefe > 4 mm (trotz optimaler Mundhygiene)
- Bei refraktärer, therapieresistenter Erwachsenen-Parodontitis
- Bei akuter, rasch verlaufender Parodontitis
- Bei Periimplantitis und vor Implantationen
Die molekulargenetische Analyse parodontopathogener Markerkeime ist heute als effizientes diagnostisches Werkzeug zur Therapieplanung und -optimierung bei Parodontal-erkrankungen anerkannt. Aufgrund seiner hohen, in zahlreichen Studien geprüften diagnostischen Qualität sind die Testsysteme micro-IDent® und micro-IDent®plus11 von Hain Lifescience die am häufigsten eingesetzten Tests in Europa.
Auf einen Blick
Molekulargenetische Testsysteme zum Nachweis von 5 bzw. 11 parodontopathogenen Markerkeimen
Ausgangsmaterial:
subgingivale Plaqueproben (abgenommen mit Papierspitzen)
DNA-Isolierung:
Methoden zur DNA-Isolierung aus Bakterien (z.B. QIAamp DNA Mini Kit der Fa. Qiagen)
Artikelnummer:
micro-IDent® (5 parodontopathogene Markerkeime)
12 Tests Art.-Nr. 232
96 Tests Art.-Nr. 23296
micro-IDent®plus11 (11 parodontopathogene Markerkeime)
12 Tests Art.-Nr. 23312
DNA•STRIP-Technologie
Downloads:
Informationsanforderung: